September 2016
____________________________________________________________________________________
Several studies across the United States and Europe found that people with HIV infection fracture their bones more than people without HIV. Research also shows that HIV-positive people have lower bone density, which can be measured by DXA scans, than people without HIV. HIV bone experts in the United States recommend DXA scans for all HIV-positive men starting at age 50 and for all women after the menopause.2
U.S. researchers working with two large HIV study groups wanted to see whether bone mineral density measured by DXA scans predicts which HIV-positive adults would later fracture a bone. They also aimed to pinpoint other factors that might predict broken bones in people with HIV infection.
How the Study Worked
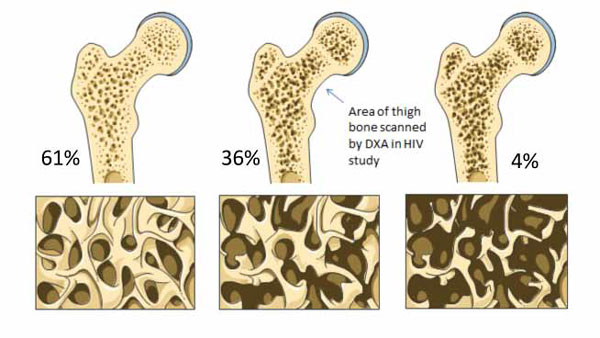
The researchers analyzed DXA bone density measurements in HIV-positive people from two U.S. groups -- the Study to Understand the Natural History of HIV/AIDS in the Era of Effective Therapy (SUN) and the HIV Outpatient Study, Denver Infectious Disease Consultants (HOPS-DIDC). Most SUN study participants had a DXA during 2004-2006, while most HOPS-DIDC participants had a DXA during 2008-2010. The research team used those scans to determine who had normal bone density, who had osteopenia (low bone density), and who had osteoporosis (very low bone density) (Figure 1). They used the standard World Health Organization definitions of osteopenia and osteoporosis based on bone density levels.| Normal Bone, Osteopenia and Osteoporosis |
 |
|
Figure 1. In a study of 1006 middle-aged people with HIV
infection, DXA scans showed normal bone in 61% (left), osteopenia in 36%
(middle), and osteoporosis in 4% (right). Darker areas in thigh bone
indicate bone loss. (Illustration from Servier PowerPoint Image Bank.) |
Then the researchers tracked people from the date of their DXA scan until (1) they had a fracture, (2) they stopped coming to study visits, or (3) a defined date in 2012. People who broke a bone before their DXA scan could participate in this analysis. The investigators used a standard statistical method to assess the impact of osteopenia or osteoporosis on having a fracture after the DXA scan. This method also identified other factors linked to a higher risk of a new fracture.
What the Study Found
The study included 1006 people, 837 of them (83%) men and 169 women. The median (midpoint) age of the study group stood at 43, and about three quarters of study participants were younger than 50. As people grow older, risk of breaking a bone because of low bone density increases. But in the general population, people under 50 rarely break bones because of low bone density.Two thirds of study participants were white, 21% were black, and 9% were Hispanic. About two thirds of the study group had become infected with HIV during sex between men. At the time of each person's DXA scan, median CD4 count stood at 461, and three quarters of the group had a viral load below 400 copies. So these people were responding well to their antiretroviral therapy. Only 12% of the study group had HCV infection, a risk factor for low bone density. But 54% of study participants smoked or used to smoke; smoking is a well-established risk factor for low bone density.3 Sixty-seven people (7%) had a fracture before their DXA scan.
Among the 1006 people studied, 611 (61%) had normal bone density near the top of the thigh bone, 358 (36%) had osteopenia, and 37 (4%) had osteoporosis (Figure 1). Blacks made up a lower proportion of those with osteoporosis (19%) than whites (57%) or Hispanics (24%). People with osteoporosis were more likely to be older, to have a lower nadir (lowest-ever) CD4 count, to have a lower body mass index (a measure of weight), to have a previous fracture, and to have HCV infection. Previous research linked all of these factors to low bone density.
Median follow-up after the first DXA scan measured 3.2 years. During that time, 85 people (8%) broke a bone. Those numbers indicate the study group had a new fracture rate of 2 per 100 person-years, meaning 2 of every 100 people broke a bone every year. Twenty-two of the 85 fractures (26%) were considered major osteoporotic fractures, that is, fractures of the hip, spine, shoulder, or forearm. Among people with new fractures, median age stood at a young 44 years, and most were younger than 50 years old.
Statistical analysis singled out two factors that predicted a new fracture regardless of whatever other risk factors a person had. Osteoporosis detected by the first DXA scan raised the risk of later fracture 4 times. And current or prior smoking raised the risk 1.59 times, that is, it raised the risk by 59%. Osteopenia did not raise the risk of a new fracture. Neither did older age, current CD4 count, lowest-ever CD4 count, HCV infection, prior fracture, or treatment with certain antiretroviral drugs linked to low bone density in previous studies.
What the Results Mean for You
This study of 1006 HIV-positive U.S. adults found that almost 1 in 10 broke a bone during 3 years of observation. The study showed that osteoporosis on a DXA scan of the thigh bone (femoral neck, Figure 1) predicts later fractures. Three quarters of people in this study, including most of those with fractures, were younger than 50 years old. Current U.S. guidelines for bone disease in people with HIV recommend DXA scans for men 50 and older and for postmenopausal women (who are usually 50 or older).2 Results of this study suggest that HIV-positive people younger than 50 may benefit from DXA scans.About 40% of people in this study had osteoporosis or osteopenia. Knowing which people already have low bone density would let HIV providers help those people take steps to avoid further bone density loss and fractures (Table 1).
The study also found that smoking makes fractures more likely. Throughout the United States and Europe, higher proportions of people with HIV than without HIV smoke. Avoiding smoking -- or quitting smoking if you have started -- can prevent not only fractures but also life-threatening heart disease, lung disease, and certain cancers. Quitting smoking usually requires a plan that your HIV provider can help you make. Such a plan often includes prescription medications such as Chantix, Zyban, or nicotine-replacement therapy. In the United States more people have quit smoking than still smoke.7
If you have osteoporosis risk factors (Table 1), talk to your HIV provider about whether you should have a DXA scan. Your provider can help you take steps to control osteoporosis risk factors that can be changed.
References
- Battalora L, Buchacz K, Armon C, et al. Low bone mineral density and risk of incident fracture in HIV-infected adults. Antiviral Ther. 2016;21:45-54.
- Brown TT, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60:1242-1251.
- Weaver CM, Gordon CM, Janz KF, et al. The National Osteoporosis Foundation's position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporosis Int. 2016;27:1281-1386.
- National Osteoporosis Foundation. Are you at risk? 2016.
- Centers for Disease Control and Prevention. Does osteoporosis run in your family? 2016.
- Mayo Clinic. Diseases and conditions: Osteoporosis risk factors. 2014.
- The Health Consequences of Smoking -- 50 Years of Progress: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.
Related Stories
Read more articles from The Body Pro, here.

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.