A Complex Interaction Resulting in Epidemiological, Clinical and Therapeutic Implications
Deborah Konopnicki; Stephane De Wit; Nathan Clumeck
______________________________________________________________
Abstract and Introduction
Abstract
HPV and HIV each display interactions favoring the other infection at the cellular level. HPV infection favors HIV acquisition in women and men, and HIV-infected individuals encompass a heavier burden of HPV-induced dysplasia and cancer due to progressive immune suppression. Both infections contribute to a vicious circle that may account for the scale-up of both pandemics in some regions of the world. HAART might be beneficial in reducing HPV infection and associated lesions, but only after several years with optimal control of HIV viremia and an immune reconstitution of great amplitude. Yet, the incidence of cervical and anal cancer has not decreased in the HAART era. In this review, we will look at the viral interactions between HPV and HIV at the cellular and clinical levels. We will analyze the epidemiological link between the two epidemics and try to propose therapeutic and vaccine strategies to act on both pandemics.
Introduction
Complex interactions between viruses have been described previously. A well-known example is the interaction between HSV infection and HIV. Genital infection with HSV significantly increases the risk of HIV acquisition. The reciprocal enhancement of viral replication leads to a worsened clinical presentation of herpes in patients with HIV as their immunity lowers, and an enhanced HIV transmission to their partners is observed in patients coinfected with herpes.
The same relations exist between HIV and HPV; the interactions start at the molecular then at the cellular level, allowing each infection to favor the acquisition and then the amplification of the other one; this then translates into clinical interactions because HPV infection and associated diseases such as warts, dysplasia and invasive cancer are enhanced by HIV coinfection, and their outcome is worsened.
In this review, we will look at the viral interactions between HPV and HIV at the cellular and clinical levels. We will analyze the epidemiological link between the two epidemics and try to propose therapeutic and vaccine strategies to act on both.
Virology
HPV is a small, nonenveloped DNA virus. Its genome is composed of E genes coding for oncoproteins and L genes coding for capsid proteins. During normal human cell replication, DNA replication errors occur frequently, leading to accumulation of the p53 protein; this protein temporarily blocks cellular replication to allow DNA repair before replication resumes. HPV oncoproteins E6 and E7 inhibit the action of p53, preventing human DNA repair; as cellular replication is no longer controlled, DNA errors and chromosomal mutations accumulate that may cause the emergence of tumor cells. HPV has the capability to escape from immune defenses, as it does not induce cellular death or viremia and when it replicates, new virions are released far from the immune system in terminally differentiated epithelial cells of the mucosa. This induces a weak or nonexistent antibody response.
There are approximately 40 different HPV genotypes affecting the human anogenital tract (cervix, vulva, vagina, penis and anus). These genotypes are divided in low-risk HPV (mostly types 6 and 11) responsible for benign warts or condylomas, which are nonmalignant tumors and high-risk (HR) HPV (mostly types 16 and 18, and less frequently types 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68) that are responsible for malignant disease. Infection with HPV is very frequent in human beings, with a lifetime infection risk of at least 80%: different type-specific HPV infections occur early during the first sexual intercourses and are transient for most individuals. However, 5–10% of women harbor persistent cervical infection with HR HPV and will thus be at risk of developing high-grade (HG) squamous intraepithelial lesions (SIL) in their third or fourth decade of life. HG SIL, also called HG dysplasia, is the stage just before cancer on cytologic samples; cervical intraepithelial neoplasia (CIN) and anal intraepithelial neoplasia (AIN) are also used to describe dysplasia on histological samples. Worldwide, the most frequent malignancy induced by HPV is invasive cervical cancer (ICC), with an incidence of 15/100,000 woman-years. Anal, penile, vaginal, vulvar and a portion of oral cancers are also induced by HPV but are less frequent in the general population with an incidence of 1–3/100,000 person-years for each different type of cancer.
HIV Favoring HPV Infection
HIV infection favors HPV at the molecular and cellular levels during the different phases of the HPV cycle, such as penetration of HPV into the target cell, HPV replication and HPV immune escape from host defenses.
In ex vivo models of oral and cervical epithelial cells in tissue explants from HIV-uninfected patients, the adjunction of HIV proteins (tat and gp120) with cytokines produced by HIV-infected cells (TNF-α and IFN-γ) has induced the disruption of epithelial tight junctions and potentiated HPV penetration into the basal epithelial cells, which are HPV targeted cells. During HPV replication, HIV tat protein was shown to significantly enhance HPV transcription and thus the expression of the HPV E oncogenes and L capsid proteins in cell cultures. To escape immune surveillance, HPV is able to induce a shift to T helper-type (Th) polarization from Th1 to Th2, with a parallel shift into cytokine production. When HIV infection progresses to AIDS, the same shift from Th1 to Th2 cytokine profile occurs in cervicovaginal secretions, and may contribute to HPV persistence.
HIV also favors HPV infection at the clinical level by increasing the new acquisition of HPV. First, HIV and HPV share a common route of transmission, such as unprotected sex with multiple partners. Second, HPV infection is further increased by progressive immune depression during HIV course. This results in HIV-infected individuals with higher HPV viral loads (VLs) than HIV-uninfected individuals, with more frequent infections with concomitant multiple HPV types, less HPV clearance and thus more frequent HPV persistent infection. Reactivation of latent HPV infection is also more frequent in HIV-positive patients with lower immunity levels. As a consequence, HPV incidence rate and prevalence is higher among HIV-infected patients. In a cohort of 652 HIV-positive women of African origin living in Europe, the incidence rate of new HR HPV infections of the cervix was 13.4, contrasting with the five per 100 woman-years found in HIV-negative women with similar age and cytology. In this study, for each increase of 100 CD4 cells/µl, there was a proportional significant decrease of the risk of carrying HR HPV with an odds ratio of 0.82 (95% CI: 0.76–0.89; p < 0.0001). Another study looking at heterosexual couples living in South Africa showed that HIV-positive status was associated with a significantly increased risk (2–3 times) of new detection of HPV in both men and women.[19] Similarly, the chance to clear HPV infection was reduced in HIV-positive men and women compared with HIV-negative men (relative risk [RR]: 0.71; 95% CI: 0.55–0.93) and women (RR: 0.46; 95% CI: 0.34–0.62).
A few studies have also found that higher HIV VL is associated with a significantly increased carriage of HPV and of SIL independently from CD4+ T-cell count decrease. HIV viremia has been shown to be an independent predictive factor for other opportunistic infections by inducing immune defects other than depletion of CD4+ T-cell count, such as cytokine production alterations. These changes are difficult to measure in daily practice but Crowley et al. compared cytokine response in cervical secretions from HIV-infected and noninfected women with and without concomitant HPV or other sexually transmitted infections (STIs). The cytokine profile was notably modified in HIV-positive patients. In another study, HIV-positive adolescents with >500 CD4+ T cells/µl had a significantly higher rate of persistent HR HPV than HIV-negative controls, illustrating that even slight changes in immune function might be responsible for higher HR HPV prevalence in HIV-positive patients. In a recent study, the risk of newly detected cervical HR HPV was increased by 2.5–5 times within 3–6 months after acquiring HIV infection. This may reflect the higher rate of HPV latent infection reactivation already demonstrated in HIV-positive patients or new HPV acquisition secondary to severe depletion of genital tract immunity immediately during acute infection as shown by previous animal models.
The prevalence of HPV anal infection also increases significantly in cases of concomitant HIV infection: HPV prevalence was 45% for any HPV genotypes and 31% for HR genotypes in 305 HIV-infected men who have sex with men (MSM) in Taiwan compared with 18% (p < 0.001) and 13%, respectively, in HIV-uninfected MSM (p < 0.001). In this study, decreasing CD4+ T-cell count was strongly associated with increasing prevalence of HPV including HR types.
Similarly to what has been largely demonstrated in the genital area, HPV infection is also more important in the oral area of HIV-infected individuals. Among 249 HIV-positive patients from Australia, HPV prevalence was 19% for all HPV genotypes and 4.4% for HPV16 compared with HPV7, and 0.8% in 251 HIV-negative patients (p < 0.001). In another study, the mean HPV VL found in saliva samples was 20-times higher in HIV-infected patients (p < 0.001).
HIV Favoring HPV-induced Lesions
HIV disease also favors the clinical manifestations of HPV-associated dysplasia, and this fact was acknowledged early in the HIV epidemics. Since 1993, ICC and HG CIN have been category C and B events, respectively, in the CDC AIDS classification. For example, the prevalence of abnormal cervical cytology is 38.3% in HIV-positive patients (HG SIL in 2.3%) compared with 16.2% in HIV-negative women (HG SIL in 1.2%) at the inclusion in the Women's Interagency HIV cohort. Ellerbrock et al. have calculated an incidence of cervical biopsy-confirmed SIL of 8.3/100 person-years in HIV-positive women compared with 1.8/100 person-years for HIV-negative women (p < 0.001). Indeed, regression of warts or SIL can be achieved by a CD4+ T-cell response against HPV antigen such as E6 and E7 oncoproteins, but this immune response is impaired during the course of HIV infection allowing HPV-associated tumors to expand. This also has an impact on the outcome after treatment of HG CIN. In a case–control study, abnormal pap smear after conization was more frequent in women with HIV (62 vs 33% in HIV-uninfected; p < 0.01) and there was HG SIL recurrence in 20% compared with none in women without HIV.
In MSM, the pooled prevalence of HG AIN proved by biopsy was 29% compared with 22% in HIV-uninfected MSM. In the same meta-analysis, anal cancer incidence was 46/100,000 HIV-positive MSM per year versus 5.1 in HIV-negative MSM. Again, there is a link with HIV-induced immune depression: the RR of anal disease progression was 2.4 in HIV-positive compared with HIV-negative MSM but it further increased to 3.1 (95% CI: 2.3–4.1) in patients with a CD4 cell count below 200/µl. However, in MSM, other factors such as increasing age, frequency of anal receptive intercourse and infection with higher numbers of HPV types are also linked with higher prevalence of HG AIN.
In a cohort of 500,000 HIV patients linked to the national US cancer registry, the incidence of cervical and anal cancer and to a lesser extent of vulvar, vaginal, penile and oral area are significantly increased in HIV-positive patients: ICC is 6–10 times more frequent than in the general population and anal cancer is 15 and 50 times more frequent in heterosexual persons and in MSM, respectively.
HPV Infection Favoring HIV Acquisition
HPV infection favoring HIV acquisition has been confirmed in several reports in women, in one study including MSM and in one trial with heterosexual men. In a recent meta-analysis combining eight studies, the risk of acquiring HIV was doubled when infection by HPV of any genotype was present prior to HIV.
Chin-Hong et al. have shown that anal infection with HPV is associated with a higher risk of HIV acquisition in MSM even after adjustment for potential confounders such as sexual activity. The risk of HIV acquisition increased significantly if there was a previous infection with two or more genotypes of HPV isolated in the same individual (hazard ratio: 3.5; 95% CI: 1.02–10.06; p = 0.002). As other ulcerative and nonulcerative STIs are known to be associated with increased HIV acquisition, HPV infection and induced lesions could disrupt the mucosal epithelia integrity allowing HIV to enter more easily. In fact, the E7 protein of HPV16 has been shown to potentiate increased permeability of genital mucosa to HIV by downregulating an epithelial adhesion molecule called E-cadherin.[40] Another assumption is that cells susceptible to HIV infection are recruited to the surface of the mucosa in cases of other concomitant STIs. The results of a case–control study following up women every 3 months in Zimbabwe are in favor of this last hypothesis. During the 22 months of follow-up, 154 women acquired HIV while 479 remained HIV-uninfected. After controlling for behavioral and biological covariates such as other STIs and use of hormonal contraception, cervical infection with HPV increased the risk of acquiring HIV infection by a 2.4-fold (95% CI: 1.5–4). This risk was enhanced with increasing numbers of HPV types isolated in the same individual. Interestingly, HIV acquisition was significantly higher in women with HPV detection loss just before acquiring HIV compared with women with persistently detectable HPV infection, with an adjusted odds ratio of 5.4 (95% CI: 2.4–9.9). This loss of HPV detection could be secondary to massive recruitment of T lymphocytes moving to the genital mucosa to eradicate HPV. These T cells are also HIV-susceptible cells and their presence could increase the target for HIV. This hypothesis has just been confirmed in a recent nested case–control study completed in heterosexual males included in a circumcision trial. HIV acquisition was linked to clearance of penile HPV secondary to an increase in epidermal dendritic cell density demonstrated by immunohistochemistry analysis in the circumcised foreskins. These dendritic cells play a central role in the cellular immune response against HPV by delivering HPV virions directly to CD4+ T cells.
Possible Epidemiological Link Between the Two Pandemics
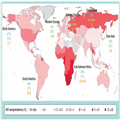
There is a lot of evidence that HIV infection enhances HPV carriage in a single individual. As a consequence, HIV also has an impact on HPV infection within couples. Among heterosexual couples living in South Africa, HIV-negative male partners of HIV-positive women had a significantly higher rate of HPV penile carriage than partners of HIV-negative females (58 vs 32%; p = 0.001). This prevalence was furthermore increased to 72% when both partners were HIV positive. Moreover type-specific sharing of HPV within the couple was also associated with HIV coinfection. This phenomenon leads to large epidemiological consequences. According to two large meta-analyses, one performed in women from the general population and the other in HIV-infected women, HPV prevalence is higher within the same region in women with HIV compared with women without HIV. When comparing the HPV infection rates and ICC incidence rates from different world regions (Figure 1), the highest prevalences are found in regions where HIV infection is more prevalent according to WHO data, such as sub-Saharan Africa.
______________________________________________________
Figure 1.
HPV infection prevalence in
the cervix and invasive cervical cancer incidence according to WHO HIV
seroprevalence distribution in 2010.
Blue statistics indicate HPV prevalence in all women. Green statistics indicate HPV prevalence in HIV-positive women. Orange statistics indicate invasive cervical cancer incidence in all women/100, 000 woman-years.6 Adapted with permission from [102].
__________________________________________________________
ICC is a major public health problem, with more than 85% of its burden occurring in developing countries. The age-standardized incidence is highest in sub-Saharan Africa and varies from 23/100,000 woman-years to 34.5 in eastern Africa compared with <10 in western Europe and North America. There are several explanations for these large differences. In most sub-Saharan African countries, ICC screening is not implemented, with less than 10% of women being screened, and vaccination against HPV is unavailable or not yet supported by a national program. At the same time HPV prevalence is much higher, and this might be a consequence of higher HIV spread in the population. A shift in HPV genotype distribution, with previously rare genotypes becoming more prevalent in the general population of some countries highly endemic for HIV in sub-Saharan Africa supports this last hypothesis. Ndiaye et al. have shown that the distribution of HR HPV genotypes found in ICC samples of 38 countries differed according to the extent of HIV infection within these countries: in countries with higher HIV seroprevalence, HR HPV types 16 and 45 were found proportionally less frequently and were replaced by type 18 in the biopsies coming from cancer centers caring for the general population.
Interaction between HIV and HPV might favor both infections in a vicious circle: HPV infection has been found to be a significant risk factor for HIV acquisition; on the other hand, HIV enhances HPV acquisition and persistence. In sub-Saharan Africa, which has the highest rates of both HIV and HPV infection worldwide, this might contribute to both HPV and HIV epidemics.
Controversies on the Role of HAART on HPV Infection & of HPV-related Lesions
Although the relationship between HIV-induced immune depletion and the burden of HPV-associated disease have been clearly demonstrated in a great body of literature, studies analyzing the effect of HAART on HR HPV infection have generated conflicting results.
In women
In a comprehensive review of the literature on cervical HPV infections and dysplasia, results on the impact of HAART on HPV disease from 22 studies published up to January 2009 were analyzed. Regarding HR HPV infection incidence, prevalence and clearance in women, the evidence coming from the older studies is inconsistent, but it was limited by a short follow-up duration of maximum 2 years after starting HAART. These studies did not measure HAART efficacy or adherence which then could be questioned; indeed, in the 1990s, HAART regimens were less well tolerated, with a higher rate of side effects and were less suitable for everyday life, with several doses per day. Looking at more recent studies (Table 1), one article concluded that there was no immediate impact of HAART on HR HPV infection, but the follow-up was only 14 months. On the contrary, four recent studies with a longer follow-up found a significant decrease in HR HPV prevalence and a better clearance 2 years after starting HAART. Fife et al. showed that decreased prevalence of HR HPV was significantly correlated with a longer follow-up. In another large cohort following 652 women for a median time of 23 months before and 38 months after entering the HPV longitudinal screening program, having an undetectable HIV VL for more than 40 months or >500 CD4+ T cells/µl for more than 18 months was independently associated with a significantly reduced risk of having an infection with HR HPV at any time during the follow-up. These results suggest that a prolonged period of optimal HIV control and an immune restoration of a large magnitude is needed before HR HPV can be cleared. This is in sharp contrast with most other opportunistic infections or HIV-related malignancies, for which the benefit of HAART can be measured within months after initiation.
Most studies published before 2009 on the incidence, progression and regression of cervical dysplasia have also yielded contradictory results, although their follow-up has been longer, at up to 4–7 years. One study that had showed a highly significant benefit of HAART on CIN incidence (hazard ratio adjusted for CD4 cell count level: 0.3; 95% CI: 0.13–0.64; p = 0.004) had followed the patients for 11 years. A more recent and larger prospective cohort found also a significantly decreased incidence and an increased regression of cervical dysplasia in South African women with HAART implemented for several years. Again there was a trend for greater protective effect of HAART proportional to longer HAART duration. The Women's Interagency HIV Study compared women to themselves before and after receiving HAART and showed a significant benefit in women adherent to their therapy. In nonadherent women there was no benefit from HAART, underlining the importance of optimal control of HIV disease to reduce HPV disease. The interesting design of this study also allowed a more precise evaluation of the possible biological effect of HAART on HPV and SIL. In contrast, other studies might have been biased by comparing women with indication for HAART, in which a more advanced disease is more probable, to women without treatment indication in which HAART is less likely to provide a benefit to HPV-associated disease outcome. HAART might also be beneficial on the outcome of dysplasia treatment. HIV-infected women who showed no recurrence of dysplasia after conization were more likely to have previously reached undetectable HIV VL (7/12, 58%) than those with recurrence (9/44, 20%; p < 0.01).
In MSM
Lower CD4+ T-cell count has been associated with an increased risk of HPV infection and with HG AIN in MSM. However, several studies looking at the impact of HAART on HPV-induced disease have also yielded conflicting results in MSM. As in women, the most recent studies seem to have a more favorable outcome, especially for patients receiving HAART for longer periods. By contrast, the early studies included fewer patients, had a shorter follow-up and did not assess HAART efficacy by HIV VL measures. Compared to women, there are much fewer studies on MSM and the number of patients enrolled is also lower, so data on MSM is still limited.
What may account for all these contradictory results? First, the important methodology discrepancies between studies make it difficult to perform comparison. Second, the population characteristics also vary between the studies: HAART-adherent versus -nonadherent patients might differ for other confounding factors such as quitting smoking or intravenous drug use, having a less risky sexual behavior; they might also be more compliant with medical follow-up and cervical or anal screening guidelines. Third, other important cofactors such as increasing age, higher frequency of receptive anal intercourses and infection by a high number of HPV types are also linked with higher prevalence of HG AIN in MSM. So if there is any benefit of HAART on anal HPV-induced disease, this benefit might be overcome by the cumulative deleterious impacts of the other concomitant cofactors. Fourth, it seems that longer duration of follow-up after HAART initiation and better-tolerated combined antiretroviral therapy (cART) regimens administered to patients included in more recent studies might account for more efficient control of HIV VL and better immune reconstitution, both leading to better control of HPV infection and induced lesions.
However, the scaling-up of cART has not been followed by a reduction of HPV-induced cancers: the incidence of cervical cancer has remained stable while it has markedly increased for anal cancer in men and women between the 1980s and 2004 in the USA and in Europe. Cumulative HPV exposure, secondary to a longer survival in HIV treated patients, is the leading hypothesis for this observation. However, the absence of decline of HPV-induced cancers with HAART might be due to more complex interactions between duration and level of both immunodeficiency and immune reconstitution. As suggested by the results of some studies, a prolonged immune restoration induced by an efficient cART after over 8 years would be needed before any improvement on HR HPV infection could be measured. As persistent HR HPV infection precedes dysplasia and then invasive cancer for 5 and 10–15 years, respectively, this might account for the high incidence of anogenital cancers despite the extent of HAART. A more recent North American cohort study compared 34,000 HIV-infected patients to 114,000 HIV-uninfected individuals between 1996 and 2007; they found that, although the risk of anal cancer in HIV-infected individuals has increased from 1996–1999 to 2000–2003, it has then stabilized in 2004–2007 for men and might even have decreased in women and heterosexual men, suggesting a delayed benefit of HAART on HPV-induced lesions. Since the recent guidelines for HIV management in the USA have changed to specify an earlier initiation of HAART, henceforth including patients with CD4+ T-cell counts superior to 350–500/µl, we will see in future studies whether earlier control of HIV viremia and maintaining a high level of immunity might translate into a clearer and more rapid benefit on HPV-induced diseases.
An issue has emerged recently regarding the impact of protease inhibitor (PI) use on HPV disease. In the D:A:D study, longer HAART exposure was associated with a lower risk of cervical cancer with an adjusted RR of 0.89 (95% CI: 0.84–0.95; p = 0.0002) per year longer exposure to PIs and 0.82 (95% CI: 0.76–0.89; p = 0.0001) for non-nucleosidic reverse transcriptase inhibitors. Surprisingly, longer PI use was associated with higher risk of anal cancer with an adjusted RR of 1.09 (95% CI: 1.04–1.14; p = 0.0003). Another very large cohort including 29,000 HIV-positive American veterans confirmed the same significant association between PI use and increased of anal cancer. A plausible biological explanation is unknown and intriguing mostly because at least one PI, that is lopinavir, has been shown in vitro to directly inhibit HPV carcinogenesis and to increase the destruction of HPV-infected cells. In a retrospective study from Germany, patients treated with a regimen including lopinavir harbored significantly less HPV infection than the other patients with other PI regimens, non-PI regimens or without therapy.
So the interactions between HAART, HPV infections and associated lesions are complex and unsolved and more data from longer prospective longitudinal cohorts are definitely needed. These studies should include HPV detection, adjustment for age and sexual activity and precise measures of the evolution of immune levels and of HIV viremia.
The Safety & Efficacy of HPV Vaccination in HIV-patients
Prophylactic Vaccines
Prophylactic vaccines against HPV are composed of virus-like particles made with synthetic L1 proteins derived from HPV6, 11, 16 and 18 that assembly together to form an empty virus-like capsid. The quadrivalent (HPV6, 11, 16 and 18) and the bivalent (HPV16 and 18) vaccines have been approved in 2007 and 2009, respectively. Both vaccines protect against HPV persistent infections and against HG AIN and CIN. The quadrivalent vaccine protects also against genital condyloma. Protection is very high for the infections and lesions induced by HPV vaccinal types, provided that the vaccine recipient has not been infected by these HPV types before vaccination. Several large randomized studies have established the safety and clinical efficacy of these two vaccines in HIV-negative adolescent girls, young women and young men including MSM.
High seroconversion rate and comparable safety profiles with the quadrivalent vaccine have been confirmed in HIV-infected children, adolescent females, women and young MSM. However, in most of these studies, the levels of antibody response were lower than in HIV-negative persons. Nevertheless the exact clinical relevance of this finding is unknown as there is no established threshold correlating with vaccine clinical efficacy. Patients receiving HAART had higher antibody response than those without HAART. The vaccination was not associated with a deleterious effect on CD4+ T-cell count or on HIV viremia. Data on the clinical efficacy against HPV-induced lesions have not yet been reported in HIV-positive patients. Data on the safety of the bivalent vaccine among HIV-positive individuals are lacking. Another concern is that the distribution of HR HPV genotypes responsible for HG AIN and CIN differ in the HIV population with more nonvaccine types found than in HIV-uninfected individuals. When analyzing the genotypes retrieved from the HG AIN biopsies from 363 HIV-infected MSM, only 56% of the patients harbored a genotype covered by the bivalent or quadrivalent vaccine; this figure drops to 45% in women according to the data from Clifford et al.. However, if we consider the future coverage by the nine-valent vaccine that will include HPV genotypes 6, 11, 16, 18, 31, 33, 45, 52 and 58, 89% of the HIV-positive patients could potentially benefit from this new vaccine currently in development in Phase III studies.
In countries such as Australia, where more than 80% of female adolescents received the vaccine, the prevalence of HPV infection and of warts caused by the vaccine genotypes has already remarkably decreased in young women 4–5 years after vaccination.
Thus, prophylactic vaccination could directly benefit HIV-infected persons if it is confirmed in ongoing efficacy trials; but it could also reduce HPV-associated infection and diseases in the HIV-uninfected population, reducing an important risk factor for HIV acquisition and spread.
Therapeutic Vaccine
Therapeutic vaccines against HPV-induced cancer are under development. They are made of long peptides from HPV16 oncoproteins E6 and E7 and they are meant to induce a strong T-cell response that would control a pre-existing tumor. In The Netherlands, a therapeutic vaccine was administered to 20 HIV-negative women with HG vulvar intraepithelial neoplasia.[81] After 12 months, 79% of the women had regression of their lesions, with a complete response in 47%. These results are remarkable mostly because vulvar intraepithelial neoplasia is frequently multifocal and conservative treatment options are very limited. A similar therapeutic vaccine was tested for safety and immunogenicity in a randomized, placebo-controlled study performed in 35 HIV-positive MSM in Australia.[82] Safety was acceptable with moderate-to-severe but short-term injection site reactions and five men had transiently detectable HIV viremia. Vaccination induced a fourfold increase in HPV16 antibody from baseline level and a threefold increase in IFN-γ response to E6 and E7 peptides in 96 and 71% of the vaccine recipients, respectively. However, after 6 months, the interferon response had fallen to prevaccination level. The study was not powered to evaluate clinical efficacy on HG AIN.
Conclusion
HPV and HIV display biological interactions favoring each infection not only in a single individual but also in couples and at the community level. This may account for a shift in HPV genotype distribution, with previously rare genotypes becoming more prevalent in the general population of some regions highly endemic for HIV like sub-Saharan Africa. HIV-infected persons encompass a heavy burden of HPV-associated disease linked mostly to progressive immune suppression. HAART is beneficial in reducing HPV infection and associated lesions, but only after several years with optimal control of viremia and a long-lasting immune reconstitution of great amplitude. Prophylactic vaccination against HPV is safe and immunogenic in HIV patients, but clinical efficacy data are pending. With regards to the high prevalence and incidence of anogenital dysplasia that remains high in HIV-infected patients despite HAART scale-up, anal and cervical cancer screening policies have to be implemented or optimized.
Future Perspective
Whether HAART will have a beneficial impact on HPV-induced cancer remains a matter of debate. A decrease in HPV-induced lesions might be achieved after several years of efficient HAART, probably in patients in whom HAART has been initiated earlier in the course of the HIV disease. However, in the significant proportion of patients diagnosed with advanced HIV diseases, the benefit of HAART on HPV disease might be overcome by a more advanced HPV disease that has been evolving for several years and for which immune reconstitution comes too late. Meanwhile, we should elucidate the possible negative impact of PI and improve cancer screening coverage in both men and women. Prophylactic vaccination by the quadrivalent vaccine, which has proved to be safe and immunogenic, should be proposed and evaluated in HIV patients until data on the bivalent and nine-valent vaccines are available. Therapeutic vaccines will probably be improved and might particularly benefit HIV-infected patients by reducing the need for recurrent or extensive excisional procedures for anogenital cancers.
Read more articles about HIV here: http://www.medscape.com




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.